A few weeks ago, I attended a live webinar event, where two well-respected dietitians discussed the use of the “low carb healthy fat” diet (LCHF) approach to help people with a range of lifestyle diseases (e.g. Diabetes) manage their health outcomes. These teams of dietitians have achieved some remarkable results with their patients, including improved glycemic control, lower blood cholesterol and better liver function test results.
There is no shortage of research suggesting that a LCHF diet may be just as effective as low-fat diets in improving metabolic risk factors, managing diabetes and reducing weight.1,2 People with insulin resistance, metabolic syndrome and type 2 Diabetes may be particularly good candidates for a lower-carbohydrate prescription, and a number of leading health organisations have come out in support of these types of diets.
 |  |
Nutrition is Not an Exact Science
Of course, like most things in nutrition science, for every body of evidence promoting a specific dietary approach, there will be research to contradict that approach. The evidence reviewed by The Institute of Medicine suggests that energy density, rather than a particular ratio of macronutrients, can lead to obesity.3 Although a high fat diet will be energy dense, the fat component alone will not lead to obesity unless energy is chronically consumed in excess of energy expenditure. This argument also applies to carbohydrates. The type of carbohydrate can also markedly influence energy density of the diet. For example, it is easier to increase the energy density of the diet by consuming energy dense drinks with added carbohydrates, compared to whole grain foods, vegetables and fruits, because the extra energy intake from the former source is generally not compensated by a reduction in energy intake from other foods. We know that there has been a major shift in westernised dietary habits over the last few decades, with an increase in consumption of highly refined carbohydrates and sugar. To add to this, less than 4% of us eat enough vegetables every day.4 This is contradictory to what dietary guidelines actually recommend.
In defence of the low-carb-healthy-fat approach that is recommended by dietitians who advocate this diet, the diet would contain a range of high quality foods (e.g. fruits, vegetables, nuts, yoghurt) that would be more nutritious than high-carbohydrate-nutrient-poor foods that are often eaten in a typical Western diet. When it comes to specific nutrients, one could even argue that the LCHF approach may not require the Recommended Dietary Intake levels (RDI) for nutrients such as thiamine, as there is less carbohydrate to metabolise. One of the presenters in the webinar has published a paper in BMJ, using a hypothetical case study design to assess the nutrient intake of a LCHF diet, and concluded that a well-planned LCHF diet would exceed the minimum nutrient reference value thresholds, except for female iron requirements, which achieved between 86-98% of the threshold. 5

But What About….?
However, as I sat watching this webinar, I couldn’t help being left pondering about the long term effects of cutting out or significantly reducing one major food group – whole grains.
We know that whole grains, one of the major food groups, are a vehicle for a range of key nutrients within the Australian diet. Take bread for example (one of the most commonly consumed whole grain foods). Bread is a major source of dietary fibre, iron, thiamine, as well as folate and iodine that has had mandatory fortification to bread making in Australia since 2009. Importantly, following folic acid fortification in Australia, there was a statistically significant 14.4% decrease in the rate of neural tube defects across the population (excluding Victoria, ACT and Tasmania where insufficient data was available).6
Whole grains feature in dietary guidelines all over the world, and with good reason. Whole grains have been linked to a lower risk of type 2 Diabetes, overweight and obesity, cancer and cardiovascular disease. 7 And whilst fruits and vegetables (part of the LCHF diet) do contain some fibre, whole grains are generally a richer source and also contain a variety of different fibre types, essential for gut and overall health.
Based on various meta-analysis, an appropriate dietary fiber intake, for example by consuming more whole grain compared to a low intake of whole grain, is linked to a significant disease risk reductions for type 2 diabetes and cardiovascular disease, 8, 9 while evidence is growing that weight management may also be supported favourably. 10.11
LCHF and the gut microbiome
Another benefit of whole grains is that they generally contain a lot of prebiotic fibres, including resistant starch, which ferments in the colon to produce short chain fatty acids that lower the PH of the colon. A lower pH has been shown to slow down the proliferation of cancer cells and decrease the production of toxic by-products.
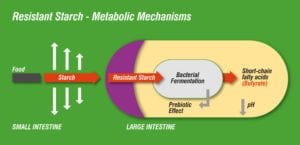
A LCHF diet will naturally be lower in prebiotic fermentable fibres compared to a higher carbohydrate diet. Given the importance of fermentable fibres to maintain a healthy and diverse gut microbiome,12 what would this mean for someone who is following the LCHF approach? Diets low in fermentable fibres have been shown to reduce total bacterial abundance,13 and this makes sense as a reduction in fermentable fibres means less-energy sources for the gut microbes, who depend on substrates to colonise? On the other hand, eating prebiotic fibres and resistant starch will allow for proliferation of intestinal bacteria, as shown in the table below. 14
Effects of non-digestable carbohydrates on gut microbiata
| Bacterial Abundance | Gene richness | Lactobacilli | Bifidobacteria | Clostridia | Enterococcus | Roseburia | Eubacteria | Ruminococcus | |
| Fibre / prebiotics | ↑ | ↑ | ↑ | ↑ | ↓ | ↑↓ | |||
| Resistant starch | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
A Grain of Truth
I certainly learned a lot from this informative webinar looking at the science underpinning the LCHF diet and how to apply in practise. There most certainly is a place for this type of diet for some individuals and any diet that gets people eating more whole foods can only be a good thing.
But for now, I think I will go and make myself a piece of whole grain toast to feed my brain and fuel my body, as I ponder where the exciting world of nutrition science will take us next!
Yours in good health,

Teri Lichtenstein, APD
The Healthy Grain Nutrition Ambassador
References:
- Hu Tian et al. Effects of Low-Carbohydrate Diets Versus Low-Fat Diets on Metabolic Risk Factors: A Meta-Analysis of Randomized Controlled Clinical Trials. American Journal of Epidemiology 2012 May; Vol. 176, No. 7
- Ajala O et al. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013;97 ;505-16
- Raynor H.A. et al. Dietary energy density and successful weight loss maintenance. Eat Behav. 2001 Apr; 12(2): 119-125
- Australian Health Survey: Consumption of food groups from the Australian Dietary Guidelines . 2011-12
- Zinn C. Rush A, Johnson R. Assessing the nutrient intake of a low-carbohydrate, high-fat (LCHF) diet: a hypothetical case study design. BMJ Open. 2018;8:e018846
- Australian Institute of Health and Welfare. Monitoring the health impacts of mandatory folic acid and iodine fortification. 2016. Available online: https://www.aihw.gov.au/reports/food-nutrition/monitoring-health-impacts-of-mandatory-folic-acid/contents/table-of-contents
- Zhang B et al. Association of whole grain intake with all-cause, cardiovascular, and cancer mortality: a systematic review anddose–response meta-analysis from prospective cohort studies. European Journal of Clinical Nutrition (2018) 72, 57–65
- Aune D et al. (2016) Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies. BMJ 353:i2716
- Ma X et al. (2016) Association between whole grain intake and all-cause mortality: a meta-analysis of cohort studies. Oncotarget 7(38):61996
- Albertson AM et al. (2016) Whole grain consumption trends and associations with body weight measures in the United States: results from the cross sectional National Health and Nutrition Examination Survey 2001–2012. Nutr J 15(1):8
- Vanegas SM et al.(2017) substituting whole grains for refined grains in a 6-wk randomized trial has a modest effect on gut microbiota and immune and inflammatory markers of healthy adults. Am J Clin Nutr 105(3):635–650
- Holscher HD. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes. 2017; 8(2): 172–184
- Halmos EP et al. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. 2015 Jan; 64(1):93-100
- Singh RK et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017; 15: 73.
Intended as general advice only. Consult your health care professional to discuss any specific concerns.





